Anatomic or non-anatomic reconstruction in patients with chronic instability of the acromioclavicular joint. What is the best approach?
Anatomic and non-anatomic reconstruction improves post-operative outcomes in chronic acromioclavicular instability: a systematic review
Francisco Xará-Leite, Renato Andrade, Pedro Silva Moreira, Luís Coutinho, Olufemi R. Ayeni, Nuno Sevivas, João Espregueira-Mendes
What did the study consist of?
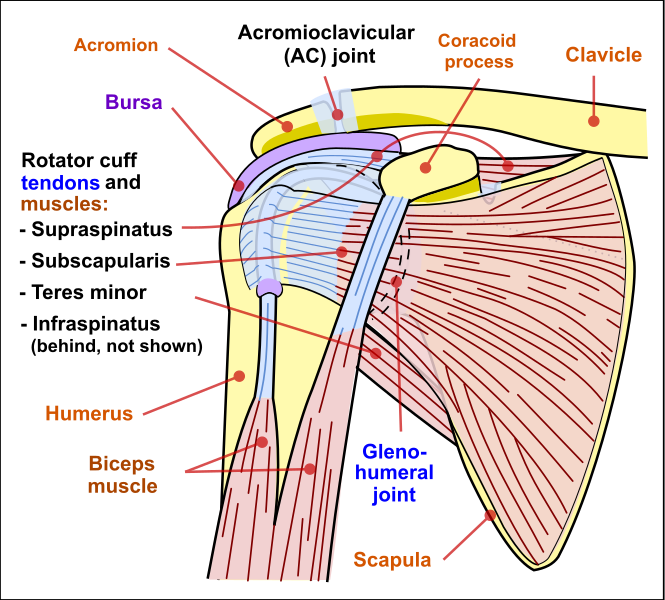
A systematic review of the literature that aimed to analyze the results of anatomic and non-anatomic reconstruction of the acromioclavicular (AC) joint in patients with chronic AC instability and determine which technique is superior.
A total of 28 studies involving 799 participants were included in the review. The anatomic reconstruction techniques included the use of tendon or synthetic grafts of autologous or allograft origin. Non-anatomic reconstructions included mostly the techniques of Weaver-Dunn or Weaver-Dunn modified.
And what results have been achieved?
- Both anatomical and non-anatomical approaches to acromionclavicular joint resulted in significant improvements in shoulder function pain in patients with chronic AC joint instability.
- The surgical failure rate was similar when using anatomic (7.5%) or non-anatomic (8.5%) reconstruction.
- Although both anatomical and non-anatomical approaches to acromionclavicular joint show positive results, comparative studies show a trend towards better results in anatomical reconstruction.
What did we learn from this work?
- Both anatomical and non-anatomical reconstructions of the acromionclavicular joint show positive results.
- A definitive conclusion as to which approach is best could not be reached.
- Until it is proven on the basis of robust scientific evidence that one approach is superior to the other, the surgeon must make the decision of which technique to use based on experience and patient preference.
Radiological and clinical outcomes.
| REFERENCE | Sub-groups | Pain (VAS) | Return to same level work | Post-op RX C-C distance | ROM (º) | |||||||||
| Pre | Post | % | Avg time (mo) | (mm) | Difference to uninjured side (mm) | |||||||||
| w/out stress | w/ stress (10kg) | w/out stress | w/ stress (10kg) | |||||||||||
| Lopez-Alameda, 2018 [28] | 1) ModWD | 6.9 | 1.8 | 96 | NR | AT | AT | AT | AT | AT | ||||
| Kocaoglu, 2017 [20] | 1) ModWD | AT | AT | AT | AT | NR | 15.6 | NR | 3.3 | AT | ||||
| 2) AUTOgraft (PL) | AT | AT | AT | AT | NR | 13.9 | NR | 1.1 | AT | |||||
| Mucciolli 2016 [30] | 1) LARS | AT | AT | NR | 5 | AT | AT | AT | ||||||
| Spencer 2016 [42] | 1) ModWD | AT | AT | AT | AT | AT | AT | AT | ||||||
| 2) ALLOgraft tunnel | AT | AT | AT | AT | AT | AT | AT | |||||||
| 3) ALLOgraft loop | AT | AT | AT | AT | AT | AT | AT | |||||||
| 4) Synthetic + ALLO loop | AT | AT | AT | AT | AT | AT | AT | |||||||
| Tauber 2016 [47] | 1) AUTOgraft (Gr, SB) | NR | 2.13 | AT | AT | NR | 13.1 ± 5.4 | NR | 6 ± 4.6 | AT | ||||
| 2) AUTOgraft (ST, TB) | NR | 0.93 | AT | AT | NR | 10.7 ± 5 | NR | 3.1 ± 3.3 | AT | |||||
| Hegazy 2016 [14] | 1) ModWD | 4.8 ± 1 | 1 ± 0.3 | AT | AT | 13.3 ± 3 | 15.9 ± 4 | NR | NR | Abd 174 ± 4, Flex 171 ± 7, RE 56 ± 9 | ||||
| 2) AUTOgraft (ST) | 4.9 ± 0.3 | 0.4 ± 0.2 | AT | AT | 11.7 ± 3 | 12.1 ± 3 | NR | NR | Abd 178 ± 2, Flex 179 ± 3, RE 66 ± 6 | |||||
| Lee 2015 [24] | 1) ModWD | AT | AT | AT | AT | NR | 11.9 | NR | 1.7 | Abd 163.5, Flex 165.7, ER 50.7, IR 73.3 | ||||
| Parnes 2015 [32] | 1) ALLOgraft (ST) | 8.1 ± 1.3 | 0.58 ± 0.79 | 100 | 6 | NR | NR | NR | 1.0 | AT | ||||
| Vitali 2015 [55] | 1) Vascular | AT | AT | AT | AT | AT | AT | AT | ||||||
| Saccomanno 2014 [38] | 1) AUTOgraft (ST) | AT | AT | AT | AT | AT | AT | AT | ||||||
| Kumar 2014 [22] | 1) ModWD | AT | AT | 100 | 3.5 | AT | AT | AT | ||||||
| 2) Surgilig | AT | AT | 100 | 1.5 | AT | AT | AT | |||||||
| Struhl 2014 [44] | 1) Double endobutton w/ continuous loop | AT | AT | AT | AT | 8.5 ± 2.4 | NR | 1.1 ± 1.2 | NR | AT | ||||
| Virtanen 2014 [54] | 1) AUTOgraft (ST & Gr) | NR | 1 ± 2 (rest)
3 ± 3 (activity) |
NR | 3.6 | AT | AT | AT | ||||||
| Wang 2014 [57] | 1) Conjoined Transfer | 4.7 | 1.2 | 100 | 3.7 | 11.4 | NR | AT | Abd 172, Flex 170, ER 56 | |||||
| Fauci 2013 [11] | 1) AUTOgraft (ST) | AT | AT | AT | AT | AT | AT | AT | ||||||
| 2) LARS | AT | AT | AT | AT | AT | AT | AT | |||||||
| Jensen 2013 [17] | 1) AUTOgraft (PL) | NR | 4.1 ± 2 | AT | AT | NR | 24.8 | 3 ± 2.3* | NR | AT | ||||
| Kim 2012 [19] | 1) ModWD | AT | AT | AT | AT | NR | 8.9 ± 1.6 | NR | NR | AT | ||||
| Windhamre 2010 [60] | 1) WD w/ PDS braid | NR | 0.7 (rest)
1 (activity) |
AT | AT | AT | AT | AT | ||||||
| 2) WD w/ hook plate | NR | 2.4 (rest)
3.7 (activity) |
AT | AT | AT | AT | AT | |||||||
| Fraschini 2010 [12] | 1) Vascular | AT | AT | AT | AT | AT | AT | AT | ||||||
| 2) LARS | AT | AT | AT | AT | AT | AT | AT | |||||||
| Boileau 2010 [5] | 1) ModWD | AT | AT | 90 | 3 | AT | AT | AT | ||||||
| Bezer 2009 [4] | 1) ModWD | AT | AT | 100 | NR | AT | AT | AT | ||||||
| Tauber 2009 [46] | 1) ModWD | AT | AT | AT | AT | 12.3 ± 4 | 14.9 ± 6 | NR | NR | Abd 171 ± 7, Flex 172.5 ± 6, RE 57 ± 7 | ||||
| 2) AUTOgraft (ST) | AT | AT | AT | AT | 11.4 ± 3 | 11.8 ± 3 | NR | NR | Abd 176 ± 4, Flex 177 ± 5, RE 63 ± 8 | |||||
| Ejam 2008 [10] | 1) Hook Plate | AT | AT | AT | AT | AT | AT | AT | ||||||
| Jeon 2007 [18] | 1) Surgilig | AT | AT | 91 | 1.25 | NR | 7 | AT | AT | |||||
| Adam 2004 [1] | 1) ModWD | AT | AT | AT | AT | AT | normal/improved (n=11, 92%), decreased (n=1, 8%) | |||||||
| Pavlik 2001 [33] | 1) ModWD | AT | AT | 94 | NR | AT | AT | AT | ||||||
| Dumontier 1995 [8] | 1) ModWD | AT | AT | 88 | NR | AT | AT | AT | ||||||
| Weinstein 1995 [59] | 1) ModWD | AT | AT | 78 | NR | AT | AT | AT | ||||||
Legend: Abd - Abduction; A-C - Acromio-Clavicular; Avg - Average; C-C - Coraco-clavicular; RE - External Rotation; Flex - Previous Flexion; Gr - Gracillis; LARS - Ligament Advanced Reinforcement System; Lig - Ligament; mo - Months; ModWD - Modified Weaver-Dunn procedure; PL - Palmaris Longus; ROM - Range Of Motion; RX - Radiological; SB - Single Bundle; ST - Semitendinous; TB - Triple Bundle; VAS - Visual Analog Scale; WD - Weaver-Dunn procedure.
This article can be found in the KSSTA journal at the link below.
Xará-Leite, F., Andrade, R., Moreira, P.S. et al. Knee Surg Sports Traumatol Arthrosc (2019).
https://doi.org/10.1007/s00167-019-05408-3
Did you know that there is a new surgical technique for the treatment of knee arthrosis? Learn more at Link

